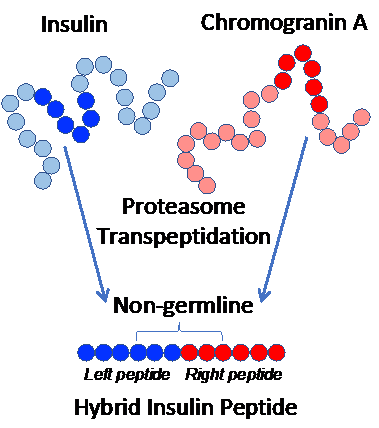
More than 1 million Americans suffer from Type 1 diabetes, which occurs when a patient’s immune T cells attack their pancreas. Understanding why this occurs is key to developing treatments that target the cause and not just the symptoms of diabetes. Recent advances by Bettini, Evavold, Liu, and colleagues showed that specific fusions/modifications between insulin and other proteins create new immunological targets that allow pathogenic high-affinity T cells to escape tolerance, destroy pancreatic beta cells, and initiate Type 1 diabetes.
References:

High self-reactivity drives T-bet and potentiates Treg function in tissue-specific autoimmunity. Sprouse ML, Scavuzzo MA, Blum S, Shevchenko I, Lee T, Makedonas G, Borowiak M, Bettini ML, Bettini M. JCI Insight. 2018 Jan;3(2). pii: 97322.

A hybrid insulin epitope maintains high 2D affinity for diabetogenic T cells in the periphery. Liu B, Hood JD, Kolawole EM, Woodruff DM, Vignali DA, Bettini M, Evavold BD. Diabetes. 2019 Dec. pii: db190399.

A critical insulin TCR contact residue selects high affinity and pathogenic insulin specific T cells. Bettini M, Scavuzzo MA, Liu B, Kolawole E, Guo L, Evavold BD, Borowiak M, Bettini ML. Diabetes. 2019 Dec. pii: db190821.